Shopping cart
Your cart empty!
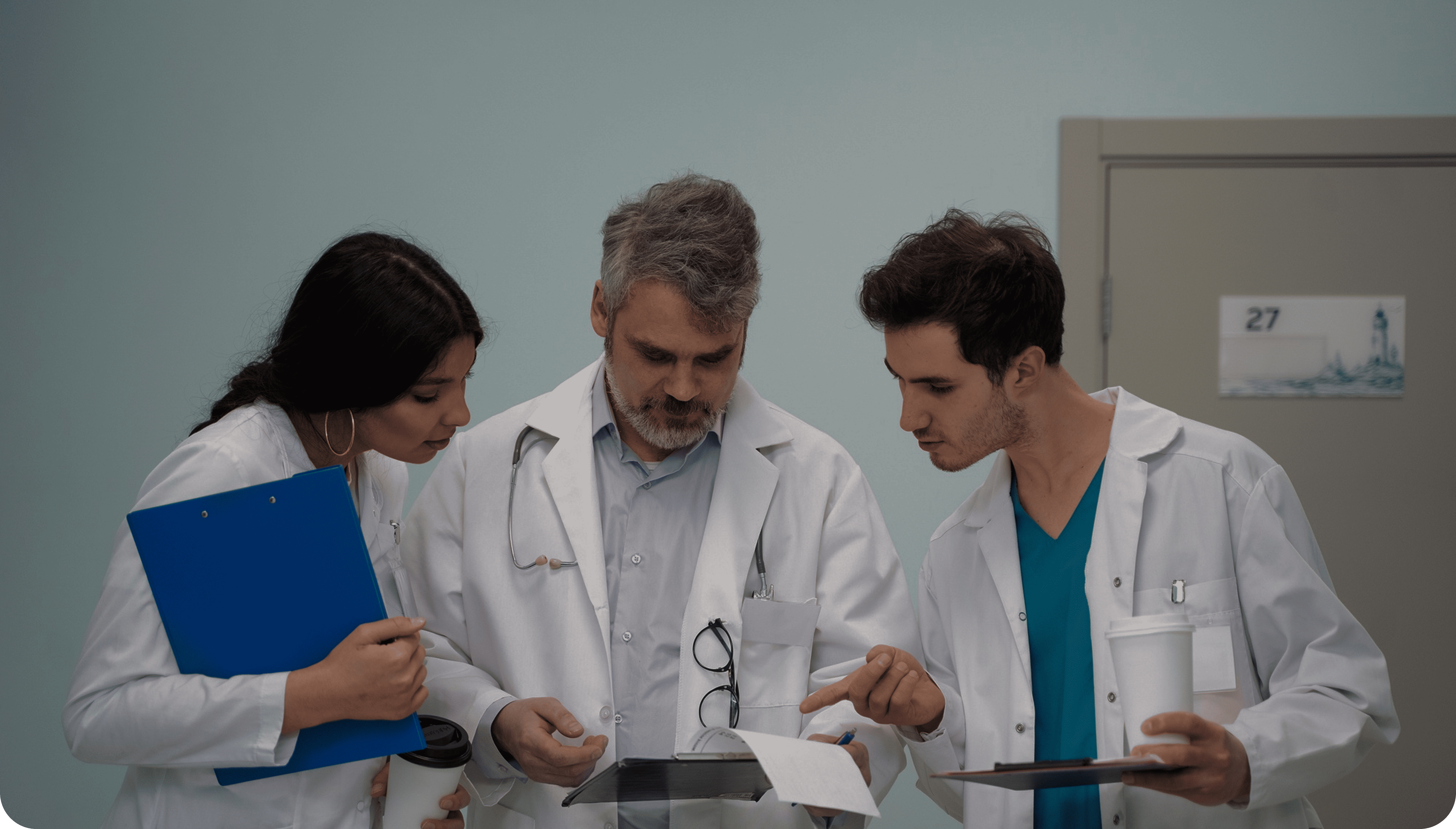
Revolutionize your outpatient operations with our tailored Ambulatory Revenue Cycle Management solutions. Leveraging advanced analytics, deep industry expertise, and a dedicated team of RCM specialists, we streamline billing processes, mitigate financial risks, and boost cash flow—allowing you to focus on delivering exceptional patient care, starting today.
Let's Talk.
Ambulatory Revenue Cycle Management (RCM) governs the financial workflows of outpatient healthcare, managing everything from patient intake to final payment. It encompasses critical functions such as billing, coding, and collections, ensuring that services are reimbursed promptly and efficiently.
Streamlined coding and billing workflows ensure your claims are approved on the first try, accelerating reimbursements.
Optimized workflows accelerate payment processing and minimize reimbursement delays, strengthening financial stability.
Efficient RCM processes cut down on administrative expenses by lessening the in-house resource burden for billing, coding, and collections.

Leverage predictive analytics to monitor reimbursement trends, identify underperforming claims, and forecast revenue.
Ambulatory outpatient practices frequently encounter significant obstacles in managing their revenue cycles: